Research On Transcendental Meditation And Ptsd
Current Multi-Site Randomized Control Trial On Meditation And Veterans With PTSD
In 2023, the David Lynch Foundation’s Institute for Mental Health and Resilience launched the largest study everTranscendental Meditation conducted on the impact of meditation on veterans and first responders with PTSD. The study is a multi-site randomized controlled trial that will evaluate whether the Transcendental Meditation (TM) technique is effective as a first-line treatment for PTSD. Secondary outcomes will include reduced depression, suicidal ideation, alcohol craving/usage, and improved sleep quality and quality of life. The 3-site study will take place at research universities around the U.S. with approximately 300 subjects. The goal of the study is to secure long-term government funding for TM.
Reference: Nidich, S., Mills, P., et al. Non trauma focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: a randomized controlled trial. The Lancet Psychiatry. 2018, 5(2), 975-986.
Results Of Clinical Trials
PTSD AND DEPRESSION SYMPTOMS
Forty veterans, diagnosed with PTSD, were assigned to TM or Treatment as Usual (TAU) control group. Participants were measured at baseline and after three months. A significant decrease in PTSD symptom severity, using the Clinician-Administered PTSD Scale (CAPS-5) was found for the TM group compared to the TAU group at three-month posttest (between group effect size Cohen’s d=0.86). Fifty percent of veterans in the TM group no longer met PTSD diagnosis at posttest, compared to 10% in the TAU group (p=.007). Significant reductions were also found for depression, anxiety, and sleep problems for the TM group compared to TAU (Cohen’s effect sizes ranged from .82 to 1.0).
Research Field Site: Northwell Health, Long Island, NY
Private foundation funding
Reference: Bellehsen, M, Stoycheva, V, et al. Transcendental Meditation as a treatment for PTSD in veterans. Journal of Traumatic Stress. 2022, 35(1), 22-31.doi.org/10.1002/jts.22665
Twenty-nine veterans were recruited into the study and taught the Transcendental Meditation program. From baseline to posttreatment, participants reported reductions in PTSD symptoms, experiential avoidance, and depressive and somatic symptoms, as well as increases on measures of mindfulness and quality of life. Gains were either maintained or continued to improve through the 2-month follow-up. Compared to baseline, EEG spectral power increased in low-frequency bands (1–7 Hz) at posttreatment and follow-up and only during meditation states suggesting TM-specific changes in brain state associated with the intervention. Following TM practice, veterans with PTSD showed improvements in PTSD symptoms, as well as increased low-frequency (1–7 Hz) EEG power that might reflect enhanced cognitive controls and internally directed attention in participants. These improvements were either maintained or continued to improve through the 2-month follow-up.
Private funding
Reference: Kang S.S., et.al. Transcendental meditation for veterans with post-traumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy. 2018 Nov;10(6):675-680. doi:10.1037/tra0000346. Epub 2018 Jul 19.
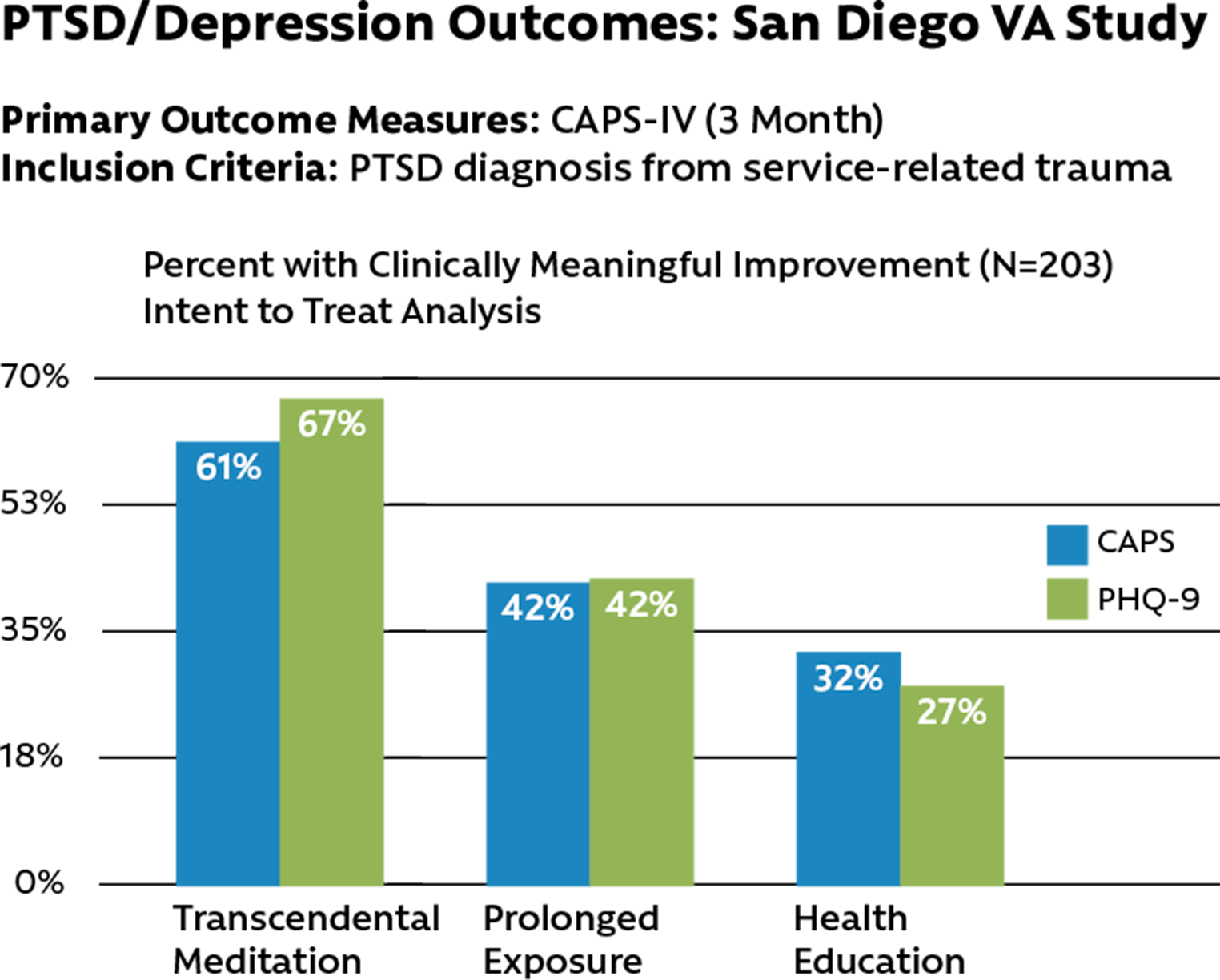
This randomized controlled study of 203 Veterans with PTSD, funded by the Department of Defense and conducted at the San Diego VA, compared the non-trauma-focused practice of Transcendental Meditation (TM) with the “gold standard” trauma-focused prolonged exposure (PE) therapy in a non-inferiority clinical trial, and compared both treatments to a PTSD health education (HE) control. For PTSD symptom severity total scores, using the Clinician-Administered PTSD Scale (CAPS-IV), both TM and PE were significantly superior to HE, with TM being non-inferior to PE over a three-month period. Similar results were found for depression using the Patient Health Questionnaire (PHQ-9). In terms of percentages of Veterans exhibiting clinically significant change on the CAPS (equal to or greater than a 10-point reduction), 61% of those receiving TM, 42% of those receiving PE, and 32% of those receiving HE showed clinically significant improvements. Results indicated the effectiveness of TM in decreasing PTSD symptom severity in Veterans and serving as an alternative for those who prefer not to receive or who do not respond to traditional exposure-based treatments of PTSD.
Research Field Site: VA San Diego
Department of Defense Grants W81XWH-12-1-0576, W81XWH-12-1-0577
Reference: Nidich, S., Mills, P., et al. Non trauma focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: a randomized controlled trial. The Lancet Psychiatry. 2018, 5(2), 975-986.
This study included 74 active military with documented PTSD or anxiety disorder not otherwise specified (ADNOS), 37 that practiced TM and 37 who did not. At 1 month, 83.7% of the TM group stabilized, decreased, or ceased medications and 10.8% increased medication dosage; compared with 59.4% of controls that showed stabilizations, decreases, or cessations; and 40.5% that increased medications (p < 0.03). A similar pattern was observed after 2 (p < 0.27), 3 (p < 0.002), and 6 months (p < 0.34). Notably, there was a 20.5% difference between groups in severity of psychological symptoms after 6 months.
Field Site: Fort Gordon, GA
Private foundation funding
Reference: Barnes V.A., et al. Transcendental Meditation and psychotropic medication use among active duty military service members with anxiety and PTSD. Military Medicine. 2016 Jan;181(1):56-63. doi: 10.7205/MILMED-D-14-00333.
Other Populations
Twenty-two female inmates at the Coffee Creek Correctional Facility in Wilsonville, OR, with at least 4 months left of incarceration were randomly assigned to either TM or a wait-list control group. Significant reductions were found over several months on total trauma symptom severity, intrusive thoughts, and hyperarousal, using the well-validated PTSD Symptoms Checklist (PCL-C). Effect sizes ranged from 0.65 to 0.99 for all variables.
Field Site: Oregon State Prison System
Private foundation funding
Reference: Nidich S., et al. Reduced trauma symptoms and perceived stress in female prison inmates through the Transcendental Meditation program: A randomized controlled trial. The Permanente Journal. 2017, 21, 16-0008.
Trauma events are four times more prevalent in inmates than in the general public and are associated with increased recidivism and other mental and physical health issues. One hundred eighty-one male prison inmates with a moderate- to high-risk criminal profile were randomly assigned to either the TM program or to a treatment-as-usual control group. The TM group compared to controls showed significant reductions in total trauma symptoms, anxiety, depression, dissociation, and sleep disturbance subscales, and perceived stress.
Field Site: Oregon State Prison System
Private foundation funding
Reference: Nidich S., O’Connor T., Rutledge T., et al. Reduced trauma symptoms and perceived stress in male prison inmates through the Transcendental Meditation program: A randomized controlled trial. The Permanente Journal. 2016, 20(4): 43-47.
This clinical trial included a total of 104 nurses at three sites, including Sarasota Memorial Hospital, Florida, randomized to either TM or usual care control groups. Measures were administered at baseline, one-month, and three-months. Results indicated significant improvements at both one-month and three-month testing periods. Three month findings showed significant decreases in PTSD symptom severity in the TM group compared to controls (p< .006; between-group effect size d=.67) and the variable of flourishing (primary outcome; p< .006; d=.65). Compliance with TM home practice was 90%.
Field Site: Sarasota Memorial Hospital
Private foundation funding
Reference: Bonamer J, Kutash M, Hartranft S, Aquino-Russell C, & Johnson A. Transcendental Meditation improves clinical nurse-well being: a multi method randomized controlled trial. Journal of Nursing Administration. 2024 54(1),16-24.
Conferences
In this virtual town hall forum, the David Lynch Foundation provides updates on some of the most exciting and inspiring achievements from our important and impactful work with Veterans, from our Resilient Warrior program.
Veterans Advisory Board








